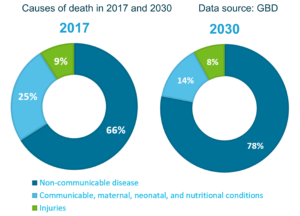
The burden of non-communicable diseases (NCD) has grown rapidly in Nepal, and contributes to two-thirds (66 %) of the total deaths that occur in the country. The majority of the NCD related deaths are attributable to the four major non communicable disease groups which are – Cardiovascular Diseases (CVDs), Cancers, Chronic Respiratory Diseases (CRD) and Diabetes. Other prevalent NCDs in Nepal include dental problems, ill mental health and road traffic injuries. In addition to large contributions in disease morbidity and mortality each year, NCDs have significant socio-economic consequences. In Nepal, 36 percent of the current total health expenditure can be attributed to NCDs.
What does this actually mean for everyday lives? It means people are living with long term health conditions that may undermine their ability to work and do everyday tasks. They are often spending substantial amount of money for treatment and management of the diseases, and they run the risk of dying earlier than the average life expectancy after acquiring NCDs. Therefore, addressing the rapidly growing burden of NCDs in Nepal and the contributing factors will help reduce these preventable deaths.
The nature of NCDs in Nepal and influential factors

Most NCDs have associated risk factors that significantly add to the burden of disease. Excessive alcohol intake, tobacco use, unhealthy diet, high consumption of salt and trans-fat and physical inactivity are the major risk factors which are behaviourally modifiable in nature. According to the WHO STEPS survey of NCD risk factors of 2019, 50 percent of Nepali men (between 15-69 years) use tobacco, whilst 97 percent of people eat insufficient serving of fruits and vegetables per day and consume nearly twice the recommended salt per day, putting Nepalis at risk of developing life-threatening chronic illnesses. Growing evidence also suggests that people living in urban areas are more likely to be overweight or obese than in rural areas, and urbanisation is associated with higher prevalence of type 2 diabetes, elevated blood pressure and increased cholesterol. Rapid and unplanned urbanisation is putting people at great risk of adopting unhealthy habits as being in the city means that fresh fruit and vegetables can be harder to access whereas high fat and sugar foods are readily available, and they are more exposed to tobacco and alcohol. Therefore, urban poor communities are more likely to be disproportionately affected by the high prevalence of NCDs.
Living with NCDs does not have an end date, it is chronic in nature which means most people will have to live with it throughout their life. Unfortunately, this also means that they will have to accrue significant financial costs for the management of those diseases. Disability is also a huge potential consequence of NCDs, which in turn affects people’s productivity and prevents them from earning money to their full potential, including money to finance the management of their health. It speaks to the importance of taking a preventable pathway to address NCDs, as cost of curative therapies might be too high for many to bear.
What are the concerns for the government in Nepal?

Government policies, programmes and strategies play important roles in improving the health and wellbeing of all citizens. The most recent National Health Policy of 2019 has focused on building an integrated health system for the prevention and management of NCDs, development of programs to promote healthy lifestyle and multi-sectoral coordination in regulation of alcohol and tobacco products. Besides that, Nepal adopted the Multi-Sectoral Action Plan for the Prevention and Control of NCDs (2014-2020) with an overall goal to reduce preventable morbidity, avoidable disability and premature mortality from NCDs. Additionally, the national plan directs the strengthening of primary health system competence to address most common NCDs among the communities. However, the multi-sectoral action plan now needs to be revised and monitored based on its goals and target. The Ministry of Health and Population (MoHP) had endorsed the WHO Package of Essential Non-communicable diseases (PEN) to enable early detection and management of CVDs, diabetes, CRDs and cancer and prevent life threatening complications such as heart attack, stroke, kidney failure, amputations and blindness. The PEN protocol 1 and 2 was introduced in July 2016 which is to be implemented in Health Post (HP) and Primary Health Care Centre (PHCC), respectively. All in all, the government has rolled out numerous policies and strategies to address growing NCDs in Nepal. It is indeed commendable and suggests that the government has strong interest in reducing the burden of NCDs in our country. Unfortunately, the results are yet to match with the efforts made.
Too many efforts from government with minimal results: What is wrong?
First, it appears the government is yet to considerably recognise the implications of our fast-growing urban population and the implications on urban health. Urban poor communities are growing in number every year in big cities of Nepal, and with low-income countries facing double burden of diseases, inevitably, vulnerable groups are most affected by this phenomenon. Urban poor households that face day-to-day hardship when they acquire any non-communicable disease because of financial difficulties. The urban poor who live in large cities with healthcare providers within their reach, will find it difficult to access these services. They may face numerous barriers such as lack of health education and information, weak financial status, long working hours and a lack of time to seek healthcare, ignorance etc. The stress of living in poverty and unstable urban neighbourhoods can mean people are more likely to smoke or consume alcohol to cope with their daily stress. Additionally, unsafe and unmanaged roads in close proximity to urban neighbourhoods can also increase the risk of traffic injuries.
The government’s initiatives towards NCD control and prevention does not take into account the unique challenges faced by urban poor or other marginalized people living in big cities. Given the growing evidence of high burden of NCDs in urban areas, national action plans should reflect the added challenge of addressing the health needs of vulnerable people in order to minimise inequity in health and healthcare services.
Concerns regarding the COVID pandemic
The COVID-19 pandemic has worsened the situation of urban poor. The COVID and the Cities report found that the government’s COVID-19 response failed to address the special needs of people living in slum settlements. The extended period of complete lockdown meant that the livelihood of daily wage earners, street vendors, poor people and people with disabilities in particular were largely affected. This can have long term consequences on the socio-economic status of already vulnerable people, which can in turn reduce their ability to seek care especially for NCD services. Moreover, the report also points out the lack of preparedness of the healthcare system to combat the pandemic which is still ongoing. Routine health services were affected including NCDs services, which can exacerbate the disease morbidity and mortality from chronic diseases.
The pandemic has revealed the vulnerabilities of already weak healthcare systems and has created the need more than ever to invest in and develop robust and resilient systems that can effectively deal with the complexities of urban poverty and the growing burden of NCDs. In order to strengthen the health system, further research will be an important step. For instance, it is important to know how health providers in cities can better meet the needs of people with NCDs and how various levels of governments can ensure healthy environments so that urban residents can avoid the risk behaviours leading to NCDs.
(The opinions expressed do not represent the views of the organization. This article has been published on https://chorusurbanhealth.org/covid-cities-blog-3rd-in-the-series/)











Comments (0)
No comments found.