In public health, Non-Communicable Diseases (NCDs) are described as being non-contagious, long-term conditions that are usually a result of genetics and lifestyle factors. Globally, the four main NCDs are cardiovascular disease, cancers, respiratory diseases and diabetes. Of all NCD deaths globally, 77% are in low and middle-income countries where prevalence is rising steadily due to changes in diet and lifestyle – changes that are fuelled by urbanisation. Providing sufficient services for patients with non-communicable diseases is a significant challenge for the health system in Nepal. Most patients, particularly in the urban context, seek care from the private sector, including hospitals, clinics, and pharmacies. However, the quality of services these facilities provide is rarely regulated or monitored and assessed within the health system. This makes it difficult to determine whether the private sector is meeting Government of Nepal standards and fulfilling patients’ needs.
Need for partnerships between public and private sectors
Public-Private Partnership (PPP) has been integrated into the national health policy as an important strategy for increased coverage and improved health outcomes. In practice, effective PPPs in Nepal are limited due to a number of challenges. Pharmacies are often perceived by the government as profit-driven enterprises rather than essential health care providers and therefore, government actors can be reluctant to work in partnership with these private providers. This can result in limited oversight by the public sector of the extent private facilities comply with registration, including renewal status, and overall quality standards. Furthermore, these facilities tend to have staff with inadequate qualifications and competencies, and they offer a limited range of services that often do not follow government health guidelines.
In general, pharmacies provide medication to their clients, both over the counter and those prescribed by doctors. Some pharmacies diagnose patients with NCDs, including diabetes and hypertension (a pre-cursor for cardiovascular disease), often without the formal training required to do so, and selling medications without prescriptions is also a common practice. Despite these issues, it is important to note that these facilities are often more readily accessible than public facilities, especially to marginalized and vulnerable populations in urban areas.
Capitalizing on the accessibility of pharmacies can support local governments to deliver NCD services to those unreached by the public health system. With the PPP concept in mind, Pokhara Metropolitan City collaborated with HERD International performed need assessment on health seeking behavior of people and health system’s readiness to explore possible PPP model in Pokhara metropolitan city.

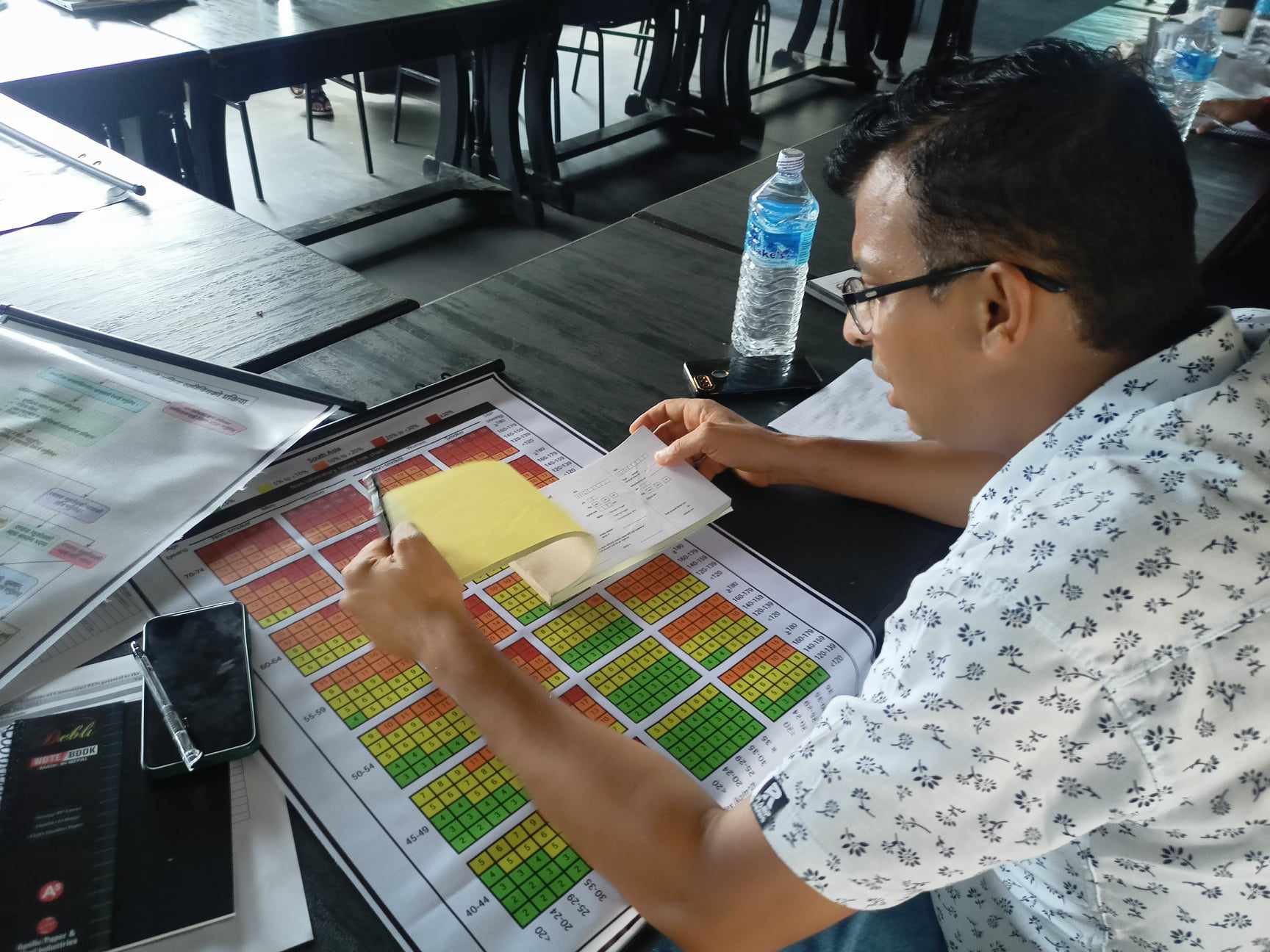
Supervision team guiding pharmacist on recording NCD register
Community perception of pharmacies: “The magic tablet”
“Where do you visit when you are sick?” HERDi researchers raised this question to a group of women in a village nestled in the southern hills of Pokhara Metropolitan City during a focused-group discussion in early 2023. Most women revealed that they visit their local health posts for common ailments such as the common cold, but they tend to visit pharmacies to seek treatment when they feel that they have more severe illnesses. One of the participants even described her local pharmacist as a magician. According to her, he provided a “jadu ko goli” (magic tablet) to cure her ailment. Other women chimed in with fervent agreement with similar anecdotes. Across several such discussions and interviews, many other participants pointed to pharmacies as being the first point of contact for health services, particularly service seekers from poorer and more vulnerable communities. The analogy of the “magic tablet” seems to represent the strong trust held by the public towards services provided by pharmacies.
To find out the service seeking behaviour of people and readiness of health system, we conducted a need assessment using both qualitative and quantitative methods. Our quantitative assessment included a survey of the readiness of 660 facilities both the public and private facilities to deliver NCD services. This included service quality, availability of NCD services and the readiness to provide them, human resources, and diagnostic service availability. We identified 352 pharmacies and they emerged as the largest providers of preliminary screening and diagnosis for diabetes and hypertension. However, their readiness scores for diabetes and hypertension services were low, at just 32 and 32.5 out of a total score of 100 respectively. Despite low readiness, pharmacies were the first point of contact for NCD care, especially among the urban poor. This was due to their proximity to people’s homes in poor neighbourhoods, their extended operating hours which allowed people to visit before and after their working day, and the fact that people felt comfortable talking about their health problems with those working in the pharmacy. Public health facilities on the other hand faced barriers such as restricted operating hours, lack of regular supply of medicines and equipment, and distance. Likewise, focus group discussions in urban slum clusters showed low awareness of NCD risks, poor compliance with treatment, misconceptions about medication, financial dependence of women on husbands, and opportunity costs linked to seeking care. Male daily wage laborers in these communities often engaged in heavy alcohol consumption, exacerbating issues such as domestic violence and health neglect.
Partnerships between public and private sectors for better health outcomes
An interesting finding emerged from our needs assessment. Despite pharmacies lacking readiness and existing absence of a referral system and patient-level record-keeping, they remained the first point of contact and the preferred providers for many. Additionally, we found that the local health system had no way of knowing the total number of patients, the types of services or treatments provided, and the medications dispensed, as pharmacies do not report to the Health Management Information System (HMIS), which is the national online repository for health data. From the private sector perspective, they feel the services they do provide are largely underappreciated and unacknowledged by the public health system, especially as they see such a large volume of patients on a near-daily basis.
Consequently, based on the evidence generated from the health facility assessments, community interviews, and co-design workshops, the Health Division of Pokhara Metropolitan City and HERDi co-designed an intervention to link pharmacies and the basic hospital in the municipality. Eleven pharmacies were requested to participate due to their status as legal pharmacies and their geographical location in proximity to poor urban neighborhoods. All 11 pharmacies were keen to be involved in the study. The co-design process resulted into a design and endorsement of a customized Package of Essential Non-Communicable Disease (PEN) as used within the national NCD guidelines to link the pharmacies to the public health system. The training on this customized PEN, was delivered by experts from the Pokhara Academy of Health Science, specifically for screening of hypertension and diabetes within the pharmacies. Key objectives included improving knowledge and skills of pharmacy staff, enhancing coordination and collaboration between the Health Division and pharmacies, including regular supervision visits to pharmacies by PMC and establishing a referral chain between the private sector and public hospitals. The pharmacies were also trained on how to maintain records for patients with hypertension and diabetes, including any referrals to public hospitals, and how to report this data to HMIS. This training was the first of its kind in Pokhara Metropolitan City, and it created a platform for both the government and the pharmacies to discuss the issues of establishing this novel linkage clearly. The Health Division Chief acknowledged that there had been no previous partnership or collaboration between the private sector, especially pharmacies, and also expressed hope that the pharmacies’ commitment to this program would provide valuable insights for future partnership endeavors.
As part of the ongoing pilot intervention, HERDi will support pharmacies in adhering to the PEN protocol through periodic follow-ups, and technical assistance as required with recording and reporting diabetes and hypertension cases and managing referrals. HERDi will also conduct joint quarterly visits to the 11 pharmacies with PEN trainers to provide refresher coaching, and support the Health Division to monitor these pharmacies through periodic visits to strengthen public-private partnerships. Additionally, HERDi will lead quarterly review meetings involving all stakeholders to track progress, discuss challenges, and determine ways forward to continue to improve services, particularly to benefit underserved urban communities.
We will conduct periodic evaluations to assess the utilization of the diabetes and hypertension service and its quality including the effectiveness of recording, reporting, and referral mechanisms. These evaluations will provide the evidence to determine the scalability of this initiative to other wards and pharmacies within Pokhara Metropolitan City and, potentially, other urban centers throughout Nepal.

PEN trainer discussing issues and ways forward with pharmacist regarding screening, recording, and referral of NCD patients.
- Photo Credit: Raju Raman Neupane and Sujan Poudel, HERD International












Comments (0)
No comments found.