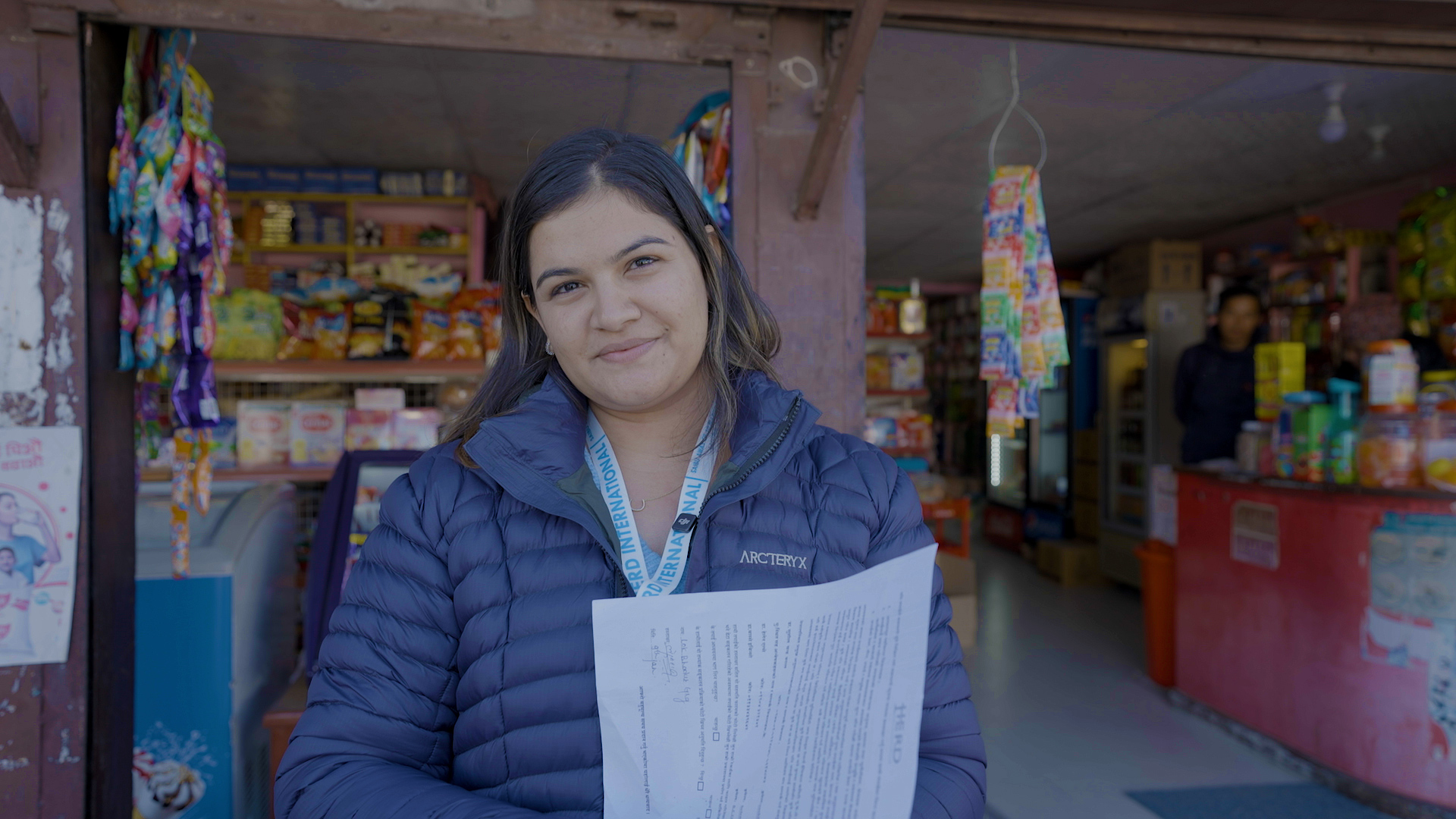
HERD International is currently implementing CARAN (Community Arts against Antibiotic Resistance in Nepal) project. It is an important project because antibiotic resistance is a growing issue in both Nepal and Worldwide. The World Health Organisation has stated that it is “one of the biggest threats to global health, food security, and development today.”
Dr Caroline Tait, Public Health Doctor, HERD International and University of Leeds talks about what are antibiotics, why are bacteria becoming resistant and what does it mean for us?
What are bacteria?
Bacteria are some of the smallest forms of life. They are too small to see with the human eye. They live all around us (including in the soil, air and water). Millions live in and on our bodies. Most are not dangerous to humans and many keep us healthy such as gut bacteria that helps us digest food. However, some cause disease such as tuberculosis, tetanus, cholera, diphtheria, gonorrhoea and urinary tract infections.
What are antibiotics?
Antibiotics are drugs used to prevent and treat infections caused by bacteria in humans and animals. They work by killing the bacteria or stopping them from multiplying. When appropriate, antibiotics must be used to cure bacterial infections. This prevents illness or death from the infection and prevents it spreading to other people. A large proportion of antibiotics taken by humans and animals pass through their systems unchanged and then enter the environment.
What is antibiotic resistance?
Antibiotic Resistance (ABR) occurs when bacteria become resistant to antibiotics. I.e. the antibiotics no longer work on that bacteria. Some people mistakenly think that people or animals become resistant to antibiotics when in fact it is the bacteria themselves that become resistant.
How do bacteria become resistant to antibiotics?
There are three ways bacteria become resistant:
- Some bacteria have natural resistance.
- Some bacteria develop resistance through their genes mutating.
- Some bacteria acquire resistance from other bacteria by sharing genes.
This occurs naturally but the use of antibiotics speeds up this process.
What are the consequences of antibiotic resistance?
When bacteria become resistant, the usual antibiotics no longer work. This means that bacterial infections may be harder to treat or – worst case-scenario – not treatable. This means people will experience more ill-health or even die from infections we used to be able to cure. They will have to stay longer in hospital, pay higher health costs and experience greater problems, such as loss of earnings. Some operations (e.g. caesarian sections), some illnesses such as immunosuppressive diseases and some treatments such as renal transplants or chemotherapy will become much more dangerous without effective antibiotics to prevent or treat infections.
Importance of addressing antibiotic use, misuse and antibiotic resistance
Tackling antibiotic misuse and ABR are global priorities. They are some of the biggest threats to global health, food security and development. ABR is rising to dangerously high levels in all parts of the world. It can affect anyone, of any age and in any country. Given the ease and frequency with which people now travel, ABR is a global problem, requiring efforts from all nations and all walks of life. ABR is a major problem now and will get worse if it is not addressed.
Research into antibiotic use, misuse and ABR such as the work being undertaken by CARAN is essential. It will help inform the local, national and global responses to tackle these issues. However, we all have a responsibility to think about and address ABR and my next blog will talk about how we can do this.









Comments (0)
No comments found.